
Disclaimer: Everything in this series of posts is YMMV (Your Mileage May Vary). I can tell you what I have experienced, read, heard, etc. but I cannot promise what it will do for you. I also don’t know your personal health history, what you already take or what you already do. If you have contraindications, I’m not the right person to recognize that and tell you. Your pharmacist and/or doctor can help you check for those before you try something.
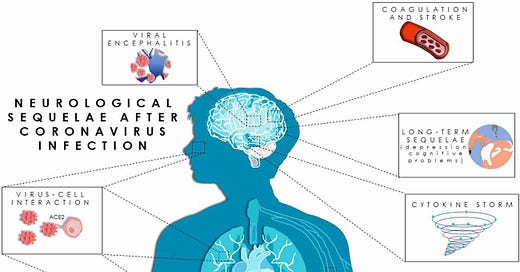
After considering the consequences of COVID for energy production, the immune system and cardiovascular system, what’s next? The brain.
Before we go into this, please be aware that I have known people who, from other diseases, had one or more elements of the types of damage COVID does. I have not been diagnosed with such damage myself, but I’m sure it happened to me too many years ago. One of my favorite authors, Elizabeth Moon, had a different type of brain injury (traumatic) and it made her unable to write any more. Over time, her ability to write returned. From all of this, I’ve seen that even if you don’t “get it all back,” the brain is marvelously adept at making workarounds for injuries which don’t fully heal.
The way new information goes into my brain is different from the way it was before my worst illness. I could feel that the way I learn changed. Decades after I got sick, I am still missing some of my IQ points. You probably can’t tell, even if you knew me before. But I am still myself and I still learn. Remember this whenever you feel alarm about what you are about to read. When I say this type of recovery is possible, I speak from personal experience and as a witness. There are moments when you need to hear that more than you need a scientific article.
UK Biobank Brain Scan Study
If you have been reading here since early on, you saw my table summarizing and translating the UK Biobank Brain Scan study findings twice in 2022. We should begin by revisiting it.
(UK Biobank Brain Scan study results, summary table by Bonnie D. Huval, ©2022)
The study was pre-print when I first noticed it. The final version of the article was posted in March 2022. Although we know more now, it is still a solid starting point for discussing what infection with SARS-CoV-2 (SARS2 for short) can do to the human brain.
In 2019 the Biobank gathered brain scans from study participants in anticipation of long term studies of the human brain over many years. After the pandemic began in 2020, the Biobank collected brain scans from study participants who got COVID. You couldn’t hope for a better setup. The scans are of the same people, shortly before and then after infection.
Note: Effects of SARS2 on the autonomic nervous system have more to do with damage to the brain stem, which is examined in other studies but not this one.
When I read the study, I saw a long list of areas of the brain that get injured. It bothered me that I didn’t understand what those areas do. For a neurologist, a blanket description of longitudinal abnormalities in limbic cortical areas with direct neuronal connectivity to the primary olfactory system means a lot. To me, it just means damage to the brain at places connected with the nose. But what does the limbic system do? It is fundamental for learning, motivation, memory (especially spatial and long term), managing emotions, processing social interactions and some behaviors essential for survival.
Rereading the study, I made a spreadsheet of the trouble areas and the type of damage found at each one. Then I read about each affected area. In the spreadsheet I included at least one link for each brain area that gives a reasonably clear picture of what it does.
Damage found in the biobank study involves areas with these responsibilities:
Cognition (thinking)
Memory
Processing of eyesight, hearing and smells
Managing the fight-or-flight response, fear and aggression
Empathy, emotional awareness and social interaction
Decision-making, goal-directed behavior, reward seeking, value-guided learning and constraining decisions to available options
Integrating prior and current information to anticipate choices
It wasn’t all about the ability to think or remember.
Such injuries can cause affected people to be more easily frustrated, frightened or angry and less able to channel their feelings appropriately. It can make them more susceptible to being manipulated by those who promote aggression as part of a push for authoritarianism. It can warp their ability to relate with and interact with other people. It can alter their self-awareness and self-control so much, it could look like a personality change.
Not everyone gets the full sweep of injury. Each person gets their own mixture in their own amounts. Such injuries are not limited to people who got severe COVID or people who develop Long COVID. Damage in the brain also occurs in people whose case felt like a common cold or even was asymptomatic.
These types of damage tend to warp your perception of your own capabilities, making it hard for you to recognize brain injury. It is often easier for someone else to deduce which parts of your brain are affected than it is for you to figure it out, but they need to know what to look for. I wouldn’t be surprised if the table helps you more in understanding what has happened to someone you know than it helps you decipher your own puzzle.
Accelerated Aging
Some studies indicate that infection with SARS2 accelerates aging.
For example, COVID survivors have shortened telomeres. Telomeres protect the ends of chromosomes. Each time a cell divides, its telomeres get shorter. Eventually the telomeres get too short for the cell to divide again. In other words, as you age, your telomeres get shorter—so when COVID shortens telomeres, it is making cells age faster.
Gene expression also shifts to what it would be at an older age. Molecular signs of premature or accelerated aging are stacking up.
Brain Fog
If you are aware that your brain isn’t behaving the way it used to, you might use the term brain fog to describe what you experience. It isn’t a proper medical term. It’s a shorthand name developed by patients with many illnesses to describe a combination of cognitive, concentration and memory issues. Decades before this pandemic, patients in the Chronic Illness forum blamed brain fog for hanging up the phone by putting it in the freezer and trying to answer the frozen peas, or coming up with bizarre wrong words, or the feeling that thinking was the mental equivalent of wading through knee-deep molasses.
Brain fog can be caused by many illnesses and mechanisms. Infection with SARS2 happens to be one of them.
Not Entirely Unique
Other viruses are known to be able to injure the brain. SARS2 isn’t even the first coronavirus to be found infecting neurons (cells in the nervous system).
According to USA NIH, the three betacoronaviruses SARS-CoV-1, MERS and SARS-CoV-2 are all associated with severe disease. The other four coronaviruses known to infect humans are generally regarded as respiratory “common cold” viruses. But two of those “no big deal” viruses are known to be able to infect the central nervous system (CNS), HCoV-229E and HCoV-OC43. The latter is associated with multiple sclerosis (MS), a disease in which the myelin sheath on CNS nerves (analogous to insulation on an electrical wire) is damaged.
Last year you may have read mainstream news claiming that Epstein Barr Virus (EBV) has been found to be the cause of MS. Always be skeptical when medical science claims EBV is the cause of a disease. It is an endemic virus carried by about 95% of adults in the Western world, often causing mononucleosis (glandular fever in the UK) during the initial acute infection. It stays in the body forever after infection. It can reactivate to cause a fresh round of symptoms when the immune system is weakened or too busy fighting something else. Reactivation in people who are already sick often tricks researchers into believing the EBV flare-up is a cause when it may be an effect. Until we learn more, saying it is associated with MS may be more appropriate than saying it is the cause.
While we are noticing that a “common cold” coronavirus is associated with MS, we should remember that MS disrupts the CNS and the brain is part of the CNS. We tend to pay attention mainly to how MS interferes with control of muscles. It can do more. A friend of a friend had photographic memory until she developed MS. She didn’t notice any other effects on her ability to use her mind, but she lost her photographic memory to MS.
Can Look Like a Psychiatric Disorder or Dementia
Not all of the effects of SARS2 on the brain produce symptoms that look like brain fog. Symptoms can come across as worsening of existing dementia (which has happened to a neighbor) or new onset of dementia. Sometimes symptoms look like a psychiatric disorder, or a well known neurological disease such as Parkinson’s.
That leads us to… tau.
Tau Proteins
Problems visible on a scan aren’t all SARS2 inflicts on the brain. According to a July 2021 article in The Lancet titled Could SARS-CoV-2 Cause Taopathy?
A large cohort study on the neurological sequelae of COVID-19 found that approximately 34% of patients received a psychiatric or neurological diagnosis within 6 months of SARS-CoV-2 infection.
Some of these diagnoses are indicative of acute or subacute changes to the CNS. Although the long-term consequences of these changes are unknown, viral infection in a subset of patients might promote chronic neuroinflammation and, over a period of years, lead to tau aggregation and neurodegeneration.
Did you notice the two headline items in this summary? They are:
In a large group of patients, SARS2 infection was followed by psychiatric or neurological trouble within a few months in about 1 out of 3 patients. That’s so high, it strongly indicates SARS2 caused the trouble.
The study points to inflammation in the brain and tau as mechanisms behind the trouble.
Tau proteins aren’t necessarily horrible. They are involved in providing structural stability for neurons and transporting nutrients. You need tau, but in the right amounts, right places and right ways.
When you have too much and it forms tangled structures or disengages from the microtubules it is supposed to help stabilize, neurological problems occur. You’re most likely to have heard of this before as one of the two most widely known hallmarks of Alzheimer’s disease. (The other hallmark is deposits of beta-amyloid protein as plaques. Abnormal tau is more strongly related to Alzheimers than plaques.) Abnormal tau is linked with other neurodegenerative diseases, too.
It's worrying to see that in this large study, so many people developed a neurological or psychiatric problem within six months after getting COVID. There are other scientific articles pointing to abnormal tau after infection with SARS2, too. However, the fact that abnormal tau has been studied for many years with other diseases gives us a jumpstart on looking for therapies.
An October 2023 review article at FrontiersIn entitled Role of Tau protein in long COVID and potential therapeutic targets discusses this. It’s a very technical article reviewing a wide swathe of studies. It makes me have to look up much of what it mentions briefly, but a few details jump out. In particular, it gives us a glimpse of how interrelated everything is. For example, I noticed mention of abnormal calcium utilization. That connects with studies of impaired cellular energy production and with Post Exertional Malaise (PEM) in myalgic encephalomyelitis (ME). It also discusses how abnormal tau promotes too much inflammation and too many cytokines.
For the brain, autonomic nervous system and peripheral nervous system, abnormal tau interferes with signaling. Neurons are all about signaling. Mess with their ability to conduct signals and everything neurons manage is affected. Cognition, memory, muscle control, autonomic functions such as heart rate, blood pressure and breathing… the whole gamut.
But the review article practically shouts that we have already learned a lot about abnormal tau. We aren’t starting from scratch.
BioMed Central published a review in October 2023 titled The therapeutic landscape of tauopathies: challenges and prospects. The bad news is that we don’t have the “magic bullet” treatment we want to see. The good news is that we do have 171 therapeutics, of which 38 are in development stages. Researchers are very busy on this and they’re getting somewhere.
Syncytial Formation
Tau is involved with structural stability, but SARS2 has other tricks up its sleeve about changing our physiological structure. SARS2 forms syncytial cells. Syncytia are created by merging cells that should remain separate. The merged syncytia do not behave the way the unmerged cells did.
You are most likely to have heard of this before in regard to Respiratory Syncytial Virus (RSV), which has been surging alongside this COVID pandemic.
Syncytial formation disrupts cellular architecture and functionality. It can lead to a cascade of events involving mitochondrial dysfunction, oxidative stress, immune system overactivation, and inflammation. Most of those categories are familiar from earlier posts in this series.
When syncytia form in the brain, neural signaling is disrupted. Combining this with mitochondrial dysfunction, oxidative stress, and abnormal tau obviously raises the risk of neurological degeneration.
What Can We Do?
Although we don’t have tidy treatment guidelines for any of this yet, we have accumulated many clues. I’ve been thinking about how narrow the clues down to just one or two paths forward that should be most likely for achieving some improvement soonest.
If I either had Long COVID or kept getting sick with everything that came by after a bout with COVID, here is what I would do, in order:
Adjust how I go about my life to reduce how many infectious diseases I have to fight off so my body can concentrate on healing what’s wrong now.
Take something (e.g. serrapeptase) to dissolve microclots unless I am reasonably certain I don’t have that problem. If I have normal d-dimer, normal clotting times, generally normal blood… then I would not need to do this.
Consider whether my symptoms suggest viral persistence. If I suspect I didn’t clear SARS2 from my body, I would pursue treatments to help me get rid of the virus. Paxlovid might not do the trick, or I might not be able to get it. In that case I would look at metformin (or berberine if I couldn’t get metformin), ensitrelvir (brand name Xocova, from Japan) if I could get any, or whichever protease inhibitors from the anti-HIV arsenal have been found most effective against SARS2 (an ever-changing list). Studies are coming out all the time with improvements to this list, so I would keep an eye open for better possibilities.
Find ways to reduce inflammation. It would probably become an ongoing quest. An awful lot of the havoc SARS2 wreaks is from overactive inflammation. Different treatments and supplements affect different aspects of inflammation, so I would expect to need to combine a few and pay attention to interactions and contraindications. I probably wouldn’t take aspirin or ibuprofen on a regular basis because those are hard on the stomach and there are gentler ways to get their anti-inflammatory effects. I might use an anti-allergy nasal spray, and take H1 and H2 antihistamines. If I’m not taking serrapeptase, I can take turmeric, for example. I might take feverfew. If my cholesterol is borderline for needing a statin to bring it down, I might ask my doctor to go ahead and try a statin without waiting for cholesterol to go higher because I have seen a study indicating statins benefit some patients with HIV and I hope it may do so after COVID, much like some other HIV therapies help (although I might not mention that motive to my doctor, depending upon my doctor’s attitude and workload).
After I got a grip on those aspects, I would start looking at what happens as we age and address such elements one at a time. There are therapeutics for cleaning out senescent cells in the brain. Dropping levels of the semi-essential amino acid taurine also occur as we age. We don’t yet fully understand how it is associated with physiological changes from organelles to organ systems, but it is. Supplementing taurine has been found to slow down DNA damage, telomerase shortening, mitochondrial impairment, and cellular senescence, so I would try taking some. I wouldn’t stop there. I would look for more possibilities like that to try, one at a time.
You can certainly make other choices. These are what I anticipate I would do. Your Mileage May Vary.
In Closing
There is no shortage of other material I could add to this series. I haven’t said anything about how SARS2 distorts the complement system (mainly because I am still learning about it), or effects on connective tissue, or the retina, or bones, or teeth… but we’ve covered enough for a reasonable foundation.
If you want more about a specific aspect of this pandemic, please tell me. Otherwise, I’d like to take a step back to my usual level of commentary on it.
Note: This post was lightly edited 2024-06-18.
—
Postscript: My 2022 posts about COVID and the brain are
Can’t Learn Anything New (2022-06-28)
The Face of Rage (2022-02-21)




I launched an experiment several years ago. I convinced my gerontology doctor to prescribe venlaflexine (Effexor xr) in increasing doses til I felt my brain fog was better. I stopped at 75 mg 2 x a day. I still am having some cognitive issues but overall it really seems to help. And I don't /have rarely felt depressed.
I also have long standing virus issues, I was diagnosed by 3 specialists in '94 (ME/CFS) ,and was able to get US SSDI, partly on brain issues. I was able to prove I had lost 20 IQ points from high school. I also take Valtrex 1 gr 2 x a day, also because I feel better on it.
I have tried both abilify and low dose naltrexone neither of which seemed to help me.