On Monday the World Health Organization updated its guidelines for handling the SARS-CoV-2 virus in laboratories. The new guidelines have sparked such an uproar, I changed my posting plans for this week to discuss it. This isn’t as hard to understand as it first appears.
How Lab Stringency in Microbe Handling is Specified
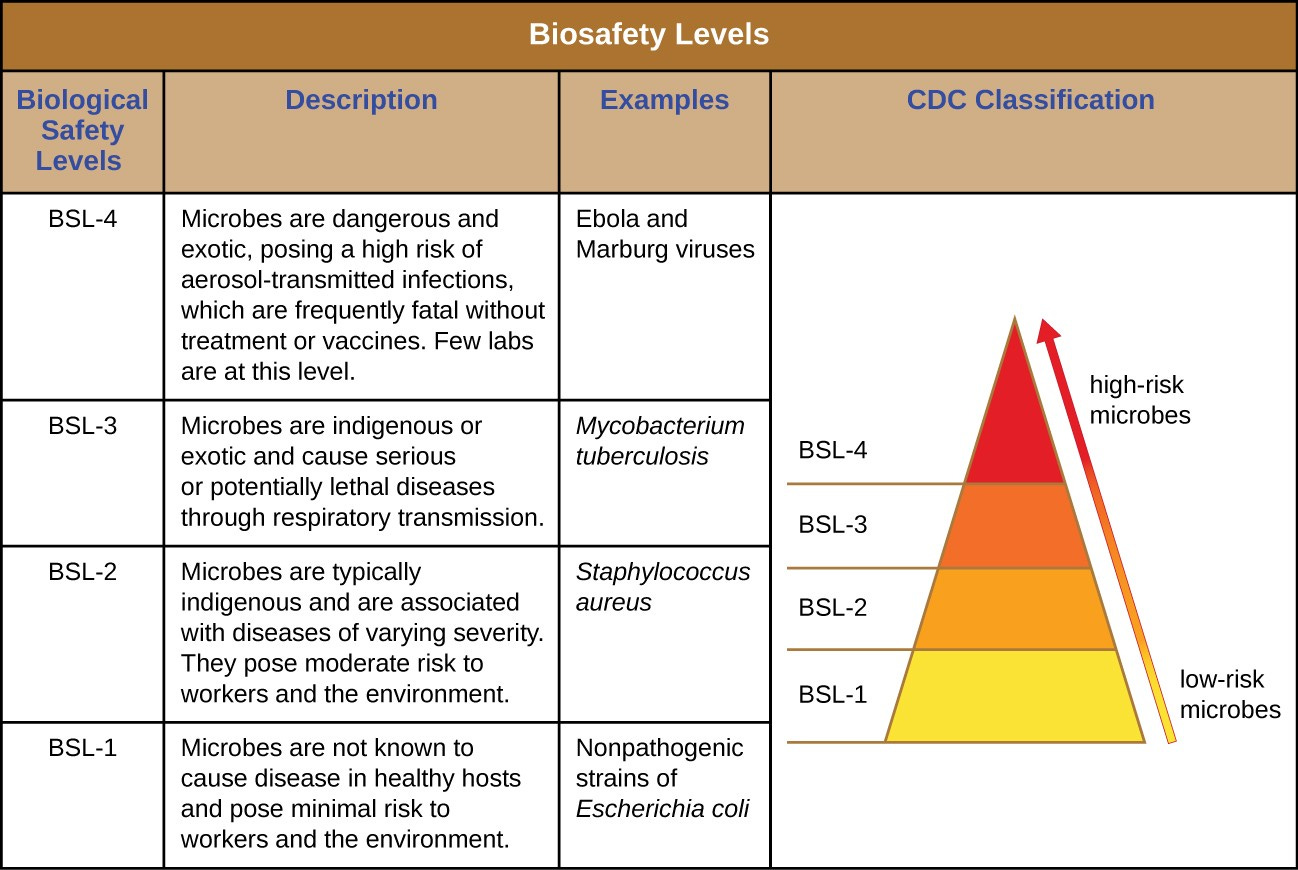
To understand what the fuss is about, we need to know there are four biosafety levels (BSLs) which lay out the way a laboratory has to be equipped and has to operate when handling microorganisms:
BSL 1 is the least stringent. This is the level of a typical high school or university laboratory. It is used for microorganisms that do not cause diseases in humans. Examples include non-pathogenic strains of E. coli and staphylococcus. (Everyone carries some of these in their bodies.)
BSL 2 is more stringent with some special equipment. It is for microbes that only cause mild disease or that are not easily spread through the air. Examples include pathogenic strains of E. coli and staphylococcus, as well as hepatitis, HIV and toxoplasma gondii. Notice that some of these cause serious disease but are handled as BSL 2 because their spread is not airborne.
BSL 3 is quite stringent with more special equipment and more protective gear for workers. It is for microbes that can spread via aerosols (airborne) and can cause severe, potentially fatal illness. Examples include tuberculosis, SARS-CoV-1, MERS-CoV, yellow fever, West Nile virus and yersinia pestis (plague, Black Death).
BSL 4 is extremely stringent, and must be. It is what you see in movies where the lab workers wear special airtight protective suits. It is for microbes that are easily transmitted, can spread via aerosols (airborne) and can cause severe, potentially fatal illness for which we have no effective vaccines or treatments. Examples include Marburg virus, Ebola virus, Lassa virus, Nipah virus and the specific Variola virus that causes smallpox.
How Did WHO Change the Rating for SARS-CoV-2?
Until Monday, SARS-CoV-2 (SARS2 for short) was a Biosafety Level 3 pathogen. Now WHO says it is BSL 2… usually.
That’s what sparked uproar.
Handling procedures less stringent than for tuberculosis seem foolish. Is that really what WHO recommends now?
In the fine print, WHO says:
Initial processing of samples should be done in a Biological Safety Cabinet or “primary containment device.”
Assays done at or near a Point Of Care (health care delivery location) can be done on a typical lab bench.
Lab work that does not involve propagating the virus should be done at BSL 2.
Lab work that does involve propagating the virus should be done at BSL 2 or higher. (More about that is in the next item.)
BSL 3 is still recommended when handling SARS2 where any of the following apply:
at high concentrations
in large volumes
from a Variant of Interest
from a Variant of Concern
from an emerging version that does not yet have a known biological profile
Practical Impact
In practice, initial processing of samples hasn’t always been getting done as carefully as WHO says it should. Assays near the point of care have been getting done the way WHO specified.
They downgraded stringency for non-propagative lab work and for some propagative work.
I’m not a public health professional or epidemiologist or virologist or medical doctor, so I don’t have authority to say this was a bad decision. I can only speak for myself.
Would I want to be responsible for that downgrade? No, I wouldn’t. Why?
SARS2 is airborne, almost as contagious as measles and tending to become more so as it evolves.
We have vaccines against it, but they are not capable of preventing people from getting infected.
Vaccines only reduce the average severity of the initial phase of an infection and reduce, to a modest degree, the likelihood of symptomatic Long COVID.
Ditto for treatments. We don’t have treatments that reliably nip infection in the bud and turn a case of COVID into a nothing-burger. We only have treatments that usually make the initial phase less severe. We do not yet know how to treat Long COVID.
Look again at the outline of what each BSL level means. This does not fit BSL 2. It fits BSL 3, at the least.
The rules to determine what BSL level applies to handling of a microorganism exist for a reason—much like launch criteria for the Space Shuttle and Spacelab missions I used to work on.
On 28 January 1986, for reasons still kept tightly sealed, someone decided not to adhere to the rules for deciding whether conditions were “go” for liftoff of a Space Shuttle mission. Challenger blew up during ascent. I remember how stricken all of us in the program felt, and how betrayed we felt later when we found out someone overrode launch criteria that day.
Downgrading SARS2 to BSL 2 for most laboratory handling elevates risk for people who operate the relevant laboratories. WHO is usually slow to declare worrisome new variants or subvariants of SARS2 as a Variant of Interest or Variant of Concern, and laboratory workers may not know whether an emerging variant is in a sample they are handling. It was safer to apply BSL 3 to all laboratory handling of SARS2 so as not to inadvertently give an especially potent flavor of it a chance to infect the lab team (and perhaps break out through them into the wider public) while WHO decides whether to tag it as especially problematic.
But I can put my reason more succinctly. Downgrading SARS2 to BSL 2 for most laboratory handling goes against WHO’s published criteria for assigning BSL levels.
I would always do everything I could to stay within launch criteria, so I would stay within the rules for assigning BSL levels. The rules exist for good reason. I wouldn’t want to be responsible, by bending them, for the next horrifying explosion.
WHO chose differently. A bunch of people would choose the way I would and that’s why so many people are so upset about the new guidelines.




What an absolute nightmare. The sheer stupidity of this decision is breathtaking, and we- the Human Race- are so screwed. And not just us, but all the animals that can be infected by it.
Excuse me, I'm going to go cry now.