Disclaimer: Everything in this series of posts is YMMV (Your Mileage May Vary). I can tell you what I have experienced, read, heard, etc. but I cannot promise what it will do for you. I also don’t know your personal health history, what you already take or what you already do. If you have contraindications, I’m not the right person to recognize that and tell you. Your pharmacist and/or doctor can help you check for those before you try something.
In After Getting COVID, Part 2, I started with a common scenario after a bout with COVID: low energy and a wonky immune system. The methodology we’re using to grapple with chronic illness (see Life with a Dratted Disease, Part 2) usually whittles away at one problem at a time, unless it’s a situation where problems are so entangled that we have to address more than one at a time or a possible solution needs all its components to have any chance of helping.
We looked at low energy first. If we dealt with the immune system first, it wouldn’t be able to do much without adequate energy.
What about the wonky immune system?
Immune System Damage
For low energy after a bout with COVID, the closest overlapping illness already “out there” is ME/CFS. Patients with ME/CFS readily share their experiences about what helps some of them, what harms them and coping strategies to help you get by.
What SARS-CoV-2 (SARS2 for short) does to the immune system is an entirely different kettle of fish. Before we look at it more closely, brace yourself. Although there is still some overlap with ME/CFS, for an essential portion of the immune system, the closest overlapping illness is better known and more widely feared. Whenever you find this overwhelming, remind yourself that unlike ME/CFS, this one is not routinely dismissed by doctors as “all in your mind.” This one shows abnormal results on some tests that your doctor can order, instead of often showing up abnormal only on tests run in research labs. This one has recognized treatments that are so effective, they can turn a dire prognosis into a chronic illness managed with medicines.
The most useful parallel for part of what SARS2 does to the immune system is HIV.
If you didn’t already know that, take a few moments to catch your breath. You may be young enough to regard HIV as a virus we can manage, but those of us who are above a certain age carry strong emotions about it as the death sentence it was for many years.
You may hear some people refer to SARS2 as airborne HIV. It isn’t.
SARS2 is indeed airborne, which makes it much easier to catch than HIV. Avoiding exposure requires a whole new set of protective measures. SARS2 is more versatile, and often sneakier, than HIV. What it does to the immune system covers a broader spectrum. But there is considerable overlap and we are more familiar with what HIV does, so we can use that to jumpstart our understanding how SARS2 bashes the immune system.
SARS2 damages the immune system in multiple ways. Depending upon the mix of those ways, it can produce a paradox. The immune system can become simultaneously weakened and overactive. When it does this, a person is more vulnerable to infection and/or cancer, and at the same time begins to have autoimmune disorders. That’s the worst combination. With some luck, you may not have that complete package of trouble.
The complete package is too much to tackle all at once. Applying our methodology again, let’s look at some of the most common portions of immune system damage one at a time.
Too Low
Many people find themselves getting new health problems after they “recover” from a bout with SARS2. I’ve put that word in quotation marks because study after study finds long term damage after acute COVID even in people who feel like they got over it and appear to be in fine health again.
Unfortunately, the immune system gets hammered by COVID. Having vital immune system components unable to work at their normal capacity (running too low) makes you vulnerable.
Lymphocytes
Lymphocytes are T-cells, B-cells and natural killer (NK) cells. They are essential warriors in the immune system, recognizing and attacking microbes and rogue cells that don’t belong. Damage to them is where HIV and SARS2 overlap.
T-cells come in multiple flavors: CD4+ (helper and regulatory) and CD8+ (cytotoxic). CD4+ cells are crucial for orchestrating the immune system. Some of them remember pathogens from an infection, which speeds up recognition and response if one of those pathogens appears again in the future. CD8+ cells attack pathogens and malignant (cancerous) cells.
B-cells create antibodies. These bind to invaders such as the SARS2 virus and neutralize them. As with CD4+ T-cells, some are memory B-cells that remember pathogens in order to respond faster if they reappear
Natural Killer (NK) cells kill cells infected by viruses, and kill cancer cells.
When your lymphocyte counts are too low, you’re extra vulnerable to opportunistic infections and some cancers, and you’re at risk for autoimmune disease.
Lymphocytopenia is a diagnostic term for not having enough lymphocytes. If you look it up in a diagnostic manual, the most common causes are:
A diet that doesn’t provide enough protein energy
Human Immunodeficiency Virus (HIV, causing AIDS)
COVID (from infection with SARS2)
Infection with certain other viruses
HIV is straightforward, killing CD4+ T-cells. You can track progression toward and through AIDS by counting how many CD4+ cells there are per milliliter of blood. As the count falls, more and more pathogens are able to take advantage of an open door no longer shielded by the group of CD4+ cells that used to guard against them.
SARS2 has a broader repertoire. It kills some CD4+ cells, makes others fight the virus until they are too exhausted to do much any more, and injures others so they don’t work properly any more. You can’t simply count cells to see how you’re doing because the cells you count may not be capable of working or may not do what they are supposed to do.
SARS2 doesn’t stop there. SARS2 causes more loss of T-cells (CD4+ and CD8+), B-cells and natural killers than HIV.
Like people with untreated HIV, you can feel like you’re okay for weeks, months, even years… but as the immune system declines, your health declines.
The next couple of paragraphs are scary.
Every new infection you catch is worse than it would be if you still had a competent immune system. Common cold, strep throat, respiratory syncytial virus, pertussis (your vaccination has probably worn off in adulthood), measles (your immunity from childhood vaccination may not still be strong enough)… anything new that you catch can take advantage of the damage SARS2 wrought to your lymphocytes. Your defenses are full of holes.
You don’t have to catch anything new to be sick a lot, either. Viruses you acquired long ago that stick around for the rest of your life and have been latent can reactivate because your immune system is no longer able to keep them suppressed. You may get shingles, which comes from reactivation of the virus that gave you chicken pox as a child. The Epstein-Barr Virus you got from some kiss or shared drink or shared ice cream spoon, probably in your teens, can wake up so you have mononucleosis (glandular fever if you’re British) that carries on and on and on. The cytomegalovirus you got in nursery school, maybe without any symptoms at the time, can flare up and cause symptoms similar to EBV or perhaps attack your central nervous system instead. Some of these viruses are in 90% to 95% of adults in the Western world. A few non-viral pathogens can lurk too, and they can reactivate when your immune system weakens. If you happen to carry latent mycobacterium tuberculosis bacteria, that can become active TB.
Remember, this is where SARS2 overlaps with HIV. There are treatments to rein in HIV.
We don’t have treatment protocols for this aspect of SARS2 yet. Some drugs that are used against HIV (mainly protease inhibitors) also show some effectiveness against SARS2. One of those drugs is part of Paxlovid™, the main treatment for initial acute COVID. We don’t know yet which of these drugs is best, or whether we need to make new drugs, or whether the specific variant(s) a person caught matters for treatment of long term effects. So… what should you do?
On behalf of your lymphocytes, play for time.
Someday there will be medications, perhaps a cocktail of a few drugs (like what happened with HIV) instead of a single drug, to help your lymphocytes recover. You want to reach that day still strong enough to get the most you can from those medications. The more you protect your lymphocytes from needing to work hard, the better they can fight both SARS2 (if it persists within you) and whatever else sneaks through or awakens, and the more intact they will be.
Too High
Discipline, coordination and good communications matter in a crisis.
Imagine Town A and Town B, each beside a river, each with a levee to protect it when the river rises unless it’s an exceptionally high flood. They have identical pump systems to lift water from the town up over the levee. They have identical trucks, stocks of bags to fill with sand, shovels and the same number of people to work on shoring up the levee in a crisis. Each town has divided its team into groups, with each group responsible for a specific portion of the levee. Each town has a reserve squad to send where a group needs reinforcements.
An exceptional flood is happening. If they add sandbags in the right places at the right times, the levee won’t be breached. But if they don’t do it right, the levee will fail and the town will suffer.
Town A’s team is a marvel of discipline. Engineers keep the pumps running. The groups listen to radio traffic and self-organize. For example, the group watching the heart section calls for materials and reserves. Everybody knows the heart section is so crucial, if it fails nothing else will matter. All the other groups do what they can to hold on with what they have. They refrain from calling for help if at all possible until the heart group announces their section is under control. Then the lung section calls for help… and so on.
No matter how frightening their situation gets, they don’t panic. The groups know their priority levels and try to ensure that materials and reserve personnel aren’t pulled in too many directions at once.
Town A’s flood defenses hold. Town A emerges intact.
Town B’s team aren’t so disciplined and level-headed. The engineers forgot to bring in extra tankers of fuel for the pump’s generators. For a while after power goes out the pumps can’t run. Water is rising in town as well as in the river. Each group only pays attention to its own situation. As the river strains the levee, the groups begin to panic.
At any given time, at least two or three groups are shouting on the radio that they need extra materials and reserve people, and their need is critical. The reserves don’t know where to go first. They are in such a rush trying to go to all the reported trouble spots, they don’t think about how rising water on the town side weakens the soil. They drive truckloads of material through the mud too close to the levee, tearing up ground that should be part of the foot of flood defences. As a result, in some places the levee starts to weaken near its base instead of only needing sandbags to extend the top. Some of the groups that call for help really could have waited or even handled their section on their own. Materials and reserve labor are wasted on their sections when they would have been more effective at another section.
Town B’s levee is breached. Town B floods.
Cytokines
When you get an infection, elements of your immune system need to communicate with each other as they defend you.
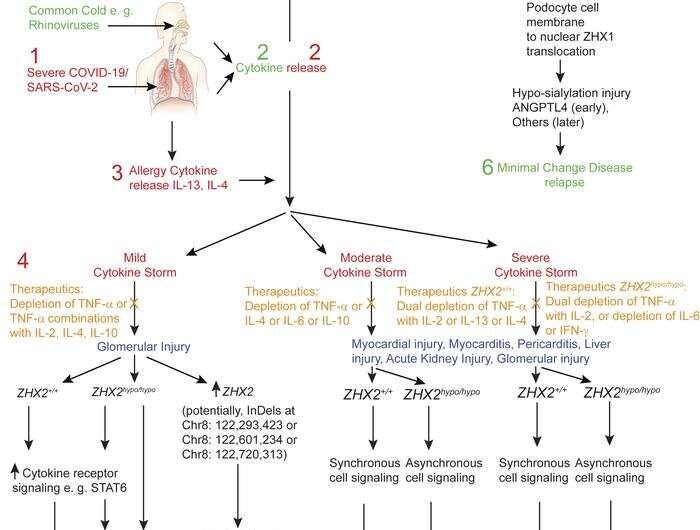
Cytokines are tiny proteins that act as molecular signals between cells. Cells in the immune system use them to communicate and coordinate, like the radio traffic in the towns facing a flood. If the immune system releases too many cytokines in its efforts to quell an invader, chaos and excessive immune system activity occur. That’s like Town B.
When this happens in the immune system, it’s called a cytokine storm. We are still trying to find ways to stop this from happening, or straighten it out after it begins to happen. People who don’t survive their bout with COVID often die from a cytokine storm.
Immune system components that become overactive (running too high) don’t just harm whatever infected you. In their confusion, they harm you too. A cytokine storm directs materials and reserves to the wrong places or to do the wrong work. Organs that haven’t been directly injured by infection can be injured by your own defense system.
Even without a cytokine storm, to fight SARS2 your body has to generate higher levels of cytokines in your body than usual. That’s part of how your body fights any infection. It’s the radio traffic your immune system uses for coordination.
Autoimmunity
Unfortunately, the cytokines don’t always step down when they should. Sometimes after part of the immune system becomes hyperactive and confused about its targeting, it forgets how to return to normal. Even after the infection is gone, the immune system is still fighting. This can turn out in any (or some mixture of) a few ways.
There’s no invader left to fight, so your immune system attacks you.
The infection never fully goes away, but it barricades itself somewhere within your body. The immune system knows it is there and strives to continue attacking it, but can’t reach it effectively. Its efforts to pierce the barricade injure you because some of your tissue is what the infection is hiding behind.
The invader displays something that looks like some of your tissues. Your immune system doesn’t realize its efforts to hit the infection also hit you.
That’s autoimmune disease. It is turning up in a disturbing proportion of people after bouts with SARS2. Autoimmune diseases we already know a lot about include multiple sclerosis (MS), systemic lupus erythematosus (SLE), Sjogren’s, scleroderma, rheumatoid arthritis… The list is long.
Although ME/CFS isn’t classified as an autoimmune disease, it often raises cytokine levels very much like what we see in Long COVID patients.
Mast Cells
Other parts of the immune system can go into overdrive and get stuck there too. For example, many people have issues after a bout with COVID that they attribute to worsened allergies. That is likely to trace to mast cells that have become overactive. (The article at the link is quite technical. To comprehend it, I have to read it slowly. But it is sufficiently detailed to help me understand the implications of some blood tests such as IgA and IgE levels. You may want to bookmark it for the same reason.)
Mast cells are considered part of the immune system, but they are also deeply involved in normal body functions. They help to regulate how dilated your blood vessels are, the growth of new blood vessels, and management of many types of specialized cells (especially but not exclusively in the immune system). They are in your connective tissue everywhere.
When mast cells are in overdrive, you have too much allergic response happening such as histamines in your system (part of the inflammatory response). As with cytokines, the right amount is helpful and too much is harmful. The term for overactive mast cells is mast cell activation syndrome (MCAS). It’s miserable. (See the link for more detail.)
What Can You Do?
I have only gone through the top headlines of what SARS2 does to our immune systems. This is enough for a starting point with your methodology for living with a chronic illness.
It would be unwise to start tinkering with your immune system before you have a reasonably clear picture of whether you have some of it running “too low” or running “too high” or a combination of both. You could take supplements that strengthen your immune system and inadvertently magnify cytokines and/or mast cell activation that’s already excessive.
Some people can paint a picture what’s happening with their immune system, at least in broad strokes, by analyzing their symptoms. That requires so much knowledge of how the body works and so much puzzle-solving, it’s very hard for most of us. Fortunately, there actually are some tools to help with this.
You can get lab tests run to provide you with genuine data about how your immune system is faring. In some countries, it is even possible to get a panel of immune system tests run by going to a lab and paying out of pocket without needing to get the tests ordered by your doctor.
You might be worried that having the results in your main medical records might have bad consequences for you such as increased premiums or coverage exclusions in your insurance. In that case, take a lesson from American AIDS patients in the 1980s and 1990s. If they had enough money to do it, they flew to Panama and paid out of pocket to have the tests done there. Results didn’t show up in their American medical records, but medical care there was American trained to CDC standards as a holdover effect of the USA’s years operating the canal there. I don’t know whether Panama is still a great place to do that. Johns Hopkins opened a medical center branch in Panama City in the mid 2000s, so there are connections into the USA’s medical records if you go to that branch. But if you go to other medical facilities in the country, maybe this approach still works.
Once you have enough data to get a sense of where your immune system isn’t right, you can look for what might help you.
Example: Inflammatory Response in Overdrive
Let’s say you see IgA, IgE, cytokine levels and other clues in your immune systems tests to indicate that whole side of your immune system—basically, your inflammatory response—is in overdrive. In particular, it looks like your mast cells are going crazy. You don’t want to stir them up any more! To start reining them in, you could start with:
H1-blocking antihistamines such as loratadine or cetirizine
H2-blocking antihistamines such as famotidine
Beclometasone sold as Beconase, Pollenase, etc.
Most escalations of treatment for MCAS will need prescriptions from your doctor and have more worrying side effects, such as corticosteroids. But your methodology involves taking a step at a time, so you can start with any of these which you can get over the counter.
You might also take action to reduce the amount of stuff you encounter that can trigger reactions from mast cells: miteproof slip covers on bed pillows under the pillowcases, an anti-allergy mattress cover under your bottom sheet, better filters in your air conditioning system or running HEPA filters in your home, and other typical steps people take to reduce their allergy symptoms.
Your general goal in this situation is to calm down the inflammatory response. If you try all of the above, one at a time, and still have too much trouble, you can borrow ideas from patients with other diseases where an overactive immune system is involved.
Here’s an unexpected clue. Many years ago, a nurse who has rheumatoid arthritis won the game show Survivor. During much of the contest, participants weren’t able to supplement their food much, so they got by on the subsistence diet of rice provided by the show. Rice is the food people are least likely to have a dietary sensitivity to, worldwide. The winner said her arthritis was better when she was “on the rice diet” during the contest. What you eat can affect how revved up your immune system is!
The Arthritis Foundation in the USA has a web page about adjusting your diet to avoid foods which can stimulate the inflammatory response. For the most part, this involves eliminating nightshade foods from your diet. It’s controversial because the medical community says there isn’t enough scientific evidence this helps. However, many rheumatoid arthritis patients say they feel better when they don’t eat nightshade foods—too many to ignore. The web page discusses how to try this dietary change to see whether it helps your inflammatory response drop down a notch.
Spices and herbs matter, not just foods.
More than 20 years ago, I read about a research team that thought people who eat cream-based curries almost every day must surely have a higher than average incidence of heart attacks and strokes. Prevailing belief at the time was that eating more fats led to higher cholesterol in the bloodstream, which deposited on the walls of arteries and led to atherosclerosis. The team studied people in India, comparing those who ate plenty of cream-based curries with those who didn’t. They thought the study would prove their theory.
It disproved their theory instead. Those who ate cream-based curries the most had the lowest incidence of heart attacks and strokes.
When the researchers delved into the situation to figure out why, the key had nothing to do with cream. The key was the turmeric in the curries. The more turmeric a person was consuming, the less likely they were to have a heart attack or stroke.
Fast forward through research a little more and the story behind arteriosclerosis becomes a tale of inflammation more than fats and oils. Scientific American brought this to my attention early on. A more recent article there walks through the highlights of how science realized inflammation is really at the core of cardiovascular disease. As one cardiologist puts it in the article, cholesterol is only some fuel and the fire is actually inflammation.
Why does this matter for you? If you can’t get a doctor to prescribe drugs to help you dial down inflammation, or if there isn’t a good drug therapy yet for the facet of inflammation causing the most aggravation, you can get spices and herbs. They may not be as effective as drugs could be, but you could find one or two that give you a little bit of improvement.
Our methodology is based on making small improvements. When we make enough small improvements, they add up, perhaps enough to make life significantly better.
Personally, for years I’ve taken turmeric and feverfew every day. That started for a specific short term reason. (I’ve mentioned this before.) I got benefits I didn’t expect and chose to continue them. For me, turmeric took two months to begin to show subtle effects I could notice. It took six months to reach full effect. Feverfew took about three days to take effect. I definitely feel the loss of either if I stop it for more than three days. Each has some anti-inflammatory effects, but in different ways. Each extends clotting time a little, so I discontinue them at least two weeks before elective surgery and don’t combine them with other “blood thinning” substances such as serrapeptase. This is a sample of the type of personal experimentation you can do on your own, looking for ways to shift your inflammatory response to a more livable level.
Solely for coping with a temporary flare-up of inflammation, Americans have over-the-counter access to an emergency way of bringing it down: DHEA and pregnenolone (not sold where I live now). These are precursor molecules used by your body in a complex chain of biochemical reactions. Outputs of this chain include estrogen, human growth hormone… and, in effect, generating your own low-dose steriods. If you take only one of the molecular supplements, you won’t get full impact. Among treatments you can give yourself, this is heavy artillery. When I first used this, it was with a doctor’s blessing but also within rules she set. It should be limited to a couple of weeks. (You shouldn’t be on steroids any more than the bare minimum.) It should also be a last resort in your personal toolkit, just to get you back to a condition you can manage with less extreme tools.
Example: Lymphocytopenia
There’s an important implication I don’t always see mentioned about lymphocytopenia. You can easily be left with an overactive inflammatory response long after any virus that triggers it seems to be gone. If your lymphocytes are getting worse, what’s killing and injuring them?
A deteriorating lymphocyte profile suggests you have viral persistence. That means SARS2 hasn’t been wiped out by your immune system. The virus may not be detectable with standard COVID tests any more, but it has set up house somewhere and your lymphocytes are among the parts of you that the virus is still attacking.
Expect to need help from a doctor in this situation. Protease inhibitors are at the leading edge of drugs that seem to do the most good. Some of the AIDS drugs (notably tenofovir, especially in the old formulation) are turning out to have some effectiveness against COVID. Research in this area is moving relatively fast, so you’ll want whatever the latest studies point to as the best option so far. You can’t get such drugs over the counter. You need a prescription. You might need to participate in a clinical trial, since there are no standard therapies for this yet.
But there are some other options. Your doctor could try prescribing drugs such as Paxlovid, metformin or remdesivir.
The digestive tract is one of the favorite places for SARS2 to lurk over the long term. The digestive tract is also entwined with the immune system. You could try to make it a less hospitable place for SARS2. How? By putting together an anecdote mentioned in the recent USA Senate hearing on Long COVID and some recent findings about probiotics.
A Long COVID patient had to undergo a colonoscopy. Preparation for that procedure involves emptying the intestines first. After the procedure, the patient took probiotics as her digestive tract began to get food into it again and her gut flora (microbiome) began to re-establish itself. She got more improvement in her health baseline from this than she had from any treatment she had tried.
This stood out. Many Long COVID patients have suspected viral persistence in their digestive tracts. Viruses are unaffected by antibiotic medications, so they have tried to use probiotics to crowd out SARS2. This doesn’t tend to go as well as what was described in the hearing. Hypothetically, emptying the gut may have left all of the microbiome starved. Repopulating it with plenty of probiotics (definitely including BLIS K12 lozenges and maybe also prebiotics) could give an advantage to the beneficial microbes and make it easier to crowd out diminished, weakened SARS2 before it has a chance to make itself a major player again.
As I said, that’s only a hypothesis, but it’s something people can approximate on their own with what they can get over the counter. Cleaning out the digestive tract is fastest when you take the vile medicine prescribed for that purpose ahead of a colonoscopy. You drink it, spend some miserable hours on the toilet and are cleaned out. But three days on a clear-liquids diet followed by less dramatic laxatives can achieve a mostly cleaned out gut.
I don’t know of anyone who has done this. If I were dreadfully sick and thought that damned virus was camping out in my digestive tract, I’d consider it. I would hope to get my doctor to collaborate with me so it would be safer, perhaps starting with a quicker and more complete cleanout made possible by the doctor’s prescriptions.
The main significance of that possible approach is the fact that it exists.
HIV persists differently. It’s hard to reach with medications. Once it is in you, we don’t have a way to get rid of it, so it’s inside forever. We can only keep it down to low levels.
But we believe SARS2 doesn’t necessarily persist after every infection, and now we have a case study that hints even persistent SARS2 may sometimes be reachable. If we can reach it, we can try to clear it out. If we can clear it out (or suppress it, as we are now able to suppress HIV), our beleagured lymphocytes can recover at least some (maybe all?) of their lost capabilities.
Last Word
Notice one more detail about that before you start planning your personal experiments to patch your immune system.
Many doctors are still in a mindset of only treating you to ease symptoms or syndromes, one issue at a time. But after a bout with COVID, you can have a wide array of problems that seem to be unrelated—at least, they would have seemed that way before this pandemic began. Now, you can consider how they may be related through damage inflicted by SARS2 and that can streamline your search for ways to get better.
You can think about what underlying damage they may have in common. Then you can address a root cause that is shared by more than one thing you are battling. Worsened allergies, catching every bug that wafts by and getting sicker than you should from it, new myocarditis, circulatory irregularities and reduced kidney function within months after a bout with COVID? Five years ago those would have seemed like separate issues. Cytokines and mast cells are involved in all of that, and we know what SARS2 can do to them—so addressing inflammation could help with the any or all of our list of new health woes.
Make of that whatever you can…
The next post in this series is After Getting COVID, Part 4.
Note: This post was edited 2024-06-18 primarily to add a paragraph about DHEA and pregnenolone.
—
Postscript: I may have to slow down on this series of posts. As we go deeper into the topic, these posts are taking more and more thought and time to write. Please forgive repetition of some snippets you have read here before. I will sometimes repeat some details to put them together with other material that is relevant.




You have invested an incredible amount of time and energy into this. I hope this can be disseminated widely. I'll have to try tumeric and feverfew for arthritic inflammation. Thanks for that tip!
Many thanks for gathering this information and writing it in a way that is easily understood.