Disclaimer: Everything in this series of posts is YMMV (Your Mileage May Vary). I can tell you what I have experienced, read, heard, etc. but I cannot promise what it will do for you. I also don’t know your personal health history, what you already take or what you already do. If you have contraindications, I’m not the right person to recognize that and tell you. Your pharmacist and/or doctor can help you check for those before you try something.
After considering the consequences of COVID for energy production and the immune system, what’s next? The cardiovascular system and perhaps a few associated bits.
Risks
In February 2022 Nature published a study showing that even a mild case of COVID-19 can increase a person’s risk of cardiovascular problems for at least a year. Although the Nature article is behind a paywall, you can read a good description of it at ArsTechnica. Researchers found that rates of many conditions, such as heart failure and stroke, were substantially higher in people who had recovered from COVID-19 than in similar people who hadn’t had the disease:
52% more likely to have a stroke
63% more likely to have a heart attack
63% more likely to develop any of 20 cardiovascular diseases
72% more likely to have heart failure
53% to 84% more likely to develop any of five types of arrhythmias
71% more likely to have atrial fibrillation
Three times the normal risk of pulmonary embolism (blood clot in a lung)
Five times the normal risk of myocarditis (inflammation of the heart muscle), which was carefully analyzed to ensure that vaccination (for which myocarditis is a rare side effect) did not contribute to the risk calculations
Risk was elevated even for those who were under 65 years of age and lacked risk factors, such as obesity or diabetes.
These figures came from people who hadn’t been vaccinated yet and hadn’t been repeatedly infected by SARS-CoV-2 (SARS2 for short). We now know that risks increase with reinfection. For people who are now on their fifth, sixth or umpteenth round with the virus, those figures are low.
Patients in the study happened to be military veterans, so their profile wasn’t representative of the general population. However, subsequent studies have found the same general pattern in more typical patient cohorts.
COVID does a lot of harm to the cardiovascular system. The harm doesn’t stop when a person seems to “recover” from their initial acute infection.
We don’t have studies saying whether the harm can always be expected to stop, and if so, when.
Signs of Damage
There are plenty of articles about abnormalities commonly found in the patients’ blood. NIH mentions several in Hematological Alterations Associated with Long COVID-19:
Low red blood cell count / low hemoglobin level. Red blood cells use hemoglobin to carry oxygen. When there are too few red blood cells (RBCs) to deliver enough oxygen throughout the body, this shows up in lab tests as low RBC count and low hemoglobin level. The result is anemia, with symptoms including fatigue and shortness of breath.
Lymphocytopenia (also called lymphopenia). This occurs when there are too few lymphocytes. The Merck Manual lists infection with SARS-CoV-2 or HIV as two of the four most common causes. See After Getting COVID, Part 3.
Thrombocytopenia. This occurs when there are too few platelets, which are also called thrombocytes. They help blood cells stick together to form clots when you need clotting to stop the bleeding at an injury. I list this here because NIH lists it, but the doctors and LC patients I watch online haven’t been talking about this. Excessive clotting is much more common with COVID.
Elevated ferritin. Long term storage of iron. High levels can produce fatigue, weakness, joint pain, belly pain, greyish or bronze skin tone, memory fog, heart problems, weight loss, hair loss or low sex drive.
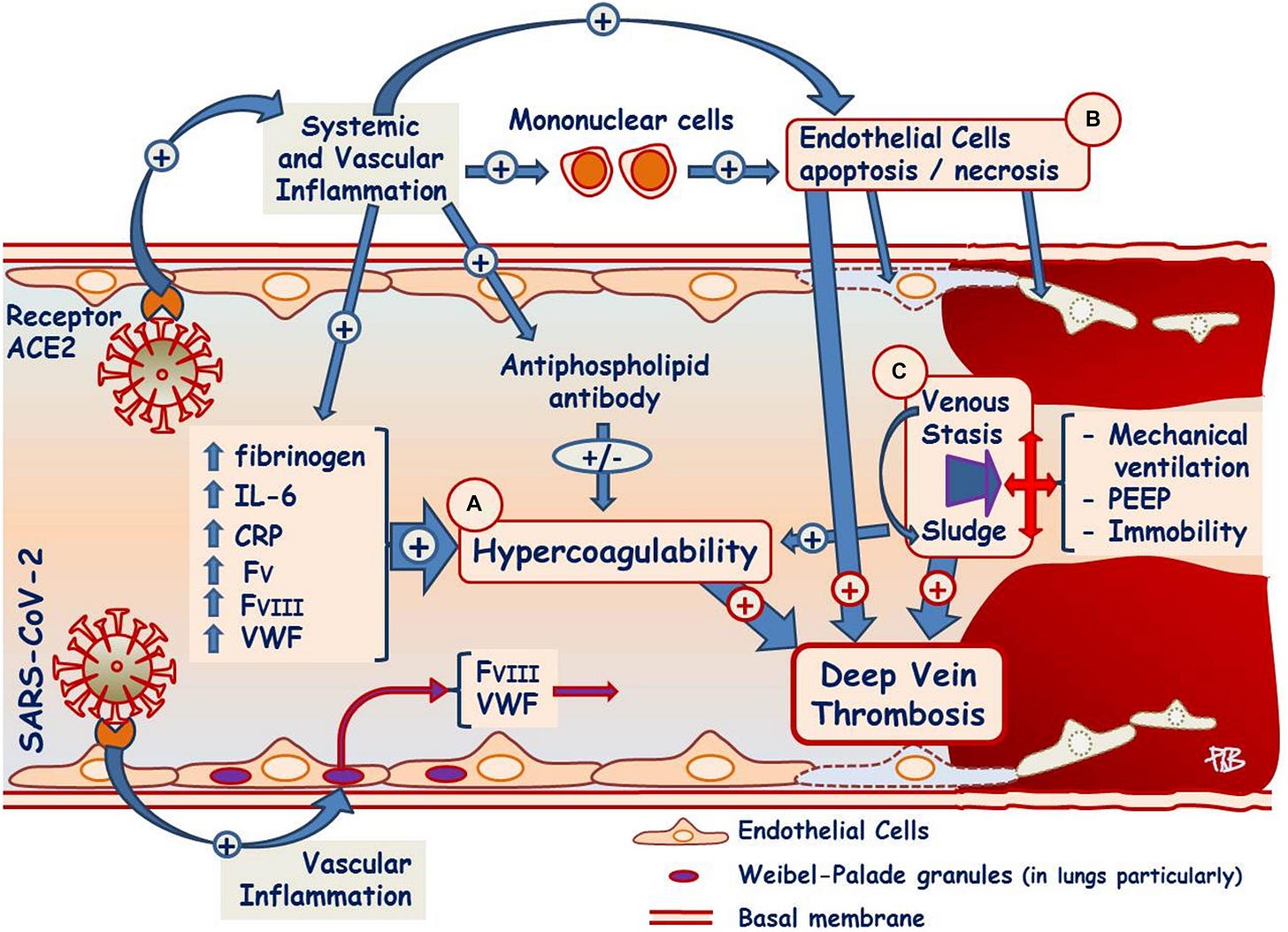
Elevated D-dimer. This protein comes from breakdown of a blood clot. Too much in the bloodstream can indicate a major clot. With COVID or Long COVID, it may indicate many fibrin amyloid microclots. Blood in COVID patients also manifests hypercoagulability (excessive inclination to clot).
Elevated interleukin-6 (IL-6). This is a cytokine, so this abnormality in blood tests indicates something happening with the immune system as discussed in Part 3 of this series.
Capillary rarefaction. Reduced density of the smallest blood vessels, a hallmark of hypertension/high blood pressure.
Although the article I cited at the top of this section is about Long COVID, other articles have pointed out the same or similar signs of damage in people who believe they recovered from COVID and may not be aware anything is wrong.
Some of these signs are relatively silent unless and until something associated with them becomes big enough to notice. It can be gradual, subtle, sudden, dramatic… If you have elevated d-dimer, it can be because you have deep vein thrombosis (DVT) which you may not even notice until the clot breaks loose and floats to your heart (heart attack) or lungs (pulmonary embolism) or brain (stroke).
If you are curious about hematology, other oddities can show up in the cardiovascular system. Postural Orthostatic Tachycardia Syndrome (POTS) is a common consequence of COVID, and involves the autonomic mechanisms that manage the cardiovascular system. Some studies have found structural changes in the heart and blood vessels as a consequence of SARS2 infection. But this list is enough to give you a starting point for checking how much your cardiovascular system has truly recovered and helping it get better if you have lasting harm.
Categories
Cardiovascular effects of COVID can be loosely grouped into a few categories:
Transport and structure
System operational management
Clotting behavior
Viral persistence
Some abnormalities show up in cardiovascular tests but are part of the immune system, such as elevated IL-6. Such items remind us that a human body is a highly complex system in which multiple subsystems work together. When we look at a subsystem, we’re simplifying our view to help us wrap our minds around what is happening, but it’s all interconnected. For immune system abnormalities that appear in cardiovascular tests, I suggest approaching them and looking for ways to treat them from the immune system angle.
Not Like Other Diseases We Know
When the consequences of a bout with COVID significantly overlap with another disease that has been around longer and is somewhat better understood, we can use the overlap to help us find ways to treat this new beast. In earlier parts of this series, we saw that a portion of the immune system damage is parallel to what HIV does. We saw that much of the hobbling of energy production is parallel to what ME/CFS does.
But claims that Long COVID is the same as ME/CFS fall apart when we look at effects on the cardiovascular system.
At first glance, there is some overlap. POTS shows up frequently in both, for example. Red blood cells that are the wrong size, shape or stiffness show up in both. This causes RBCs not to pass through capillaries the way they should, impeding blood flow and thereby impeding delivery of oxygen to tissues.
But ME/CFS patients also often have low blood volume, which I have not seen reported after bouts with COVID. My household is experiencing a real-life demonstration of the implications. New housing developments are being built in our village, but the water supply has not been increased. When we open a faucet, we don’t get as much water flow as we used to because not as much water reaches our part of the village. It takes longer to fill the kettle. In a person with low blood volume, it takes longer to fill chambers in the heart—and the blood is thicker, so it doesn’t flow as easily as it should.
That may be related to ME/CFS patients having a heartbeat pattern that doesn’t fill the ventricles (large pumping chambers) as much as normal before each pumping beat. The heart tries to compensate by squeezing harder. It’s exhausting, doesn’t pump blood as efficiently as normal and can gradually result in some enlargement of the heart. I have not seen low blood volume or this oddity of heart function described in studies of COVID or Long COVID patients.
When we look at clotting behavior and in some people indications of SARS2 viral persistence, it becomes crystal clear that ME/CFS is inadequate as a possible model of what’s going on. Cardiovascular effects of COVID are, as a package, new territory.
Figuring Out What’s Going On
The most important question to ask about your personal cardiovascular situation during and after a bout with COVID is:
Does it look like SARS-CoV-2 has not been cleared out of your body?
If SARS2 has established a reservoir for itself, treating symptoms will always be an uphill battle. You could beat back a symptom and the virus will create a new one. The longer the virus stays within you, the more opportunity it has to dig itself in and establish barricades against your immune system and against anything you take to try to attack it.
If you have viral persistence, the golden ticket for you is to somehow kick the virus out of your body. Once it is gone, you can work on healing the injuries it inflicted by treating symptoms, typically one at a time, and the virus will no longer be creating new problems so you can actually make some gains.
After the initial acute infection, you aren’t likely to be able to detect the virus with rapid or PCR tests unless its reservoir is readily accessible. When it makes itself at home in the digestive tract, sometimes people detect it by testing their poo. But if it makes itself at home in your liver, heart, kidney, brain—any of several organ systems you can’t reach—it will only be found by tests run on tissue from a biopsy. We know that it does set up reservoirs in such places because autopsies have found it in such places.
When you can’t reach it for testing, you have to analyze what’s happening to you and deduce whether viral persistence is likely to be involved.
How can you do that? Nobody has a proper answer to that question yet, but from our methodology we have some ideas.
In the U.S. Senate hearing about Long COVID, one of the witnesses was the mother of a young woman with serious LC. The young woman’s symptoms include significant gastrointestinal issues. At some point she had to get a colonoscopy. Clearing out the intestines is necessary before the procedure. After the colonoscopy, she took some probiotics as she got to eat again and refill her gut.
Her LC got substantially better.
Her experience strongly suggests SARS2 was lurking in her digestive tract. She inadvertently knocked it down and helped her system repopulate with a better microbiome.
It’s a great example of getting better from something other than a magic pill.
If your mix of symptoms suggests SARS2 is still in you, think about where it may be lurking. Then think about whether there is some way you can disrupt it. Look at what LC patients with similar symptoms have done that was helpful for them.
Make sure to investigate before you try something yourself. Whatever you try needs to make logical sense, not put you at undue risk of dangerous side effects, have no important contraindications for you (e.g. not be risky with some feature of your personal health history) and have no bad interactions with anything else you are taking or eating. (All of this applies whether you are trying to get rid of viral persistence or “only” trying to whittle down some of your symptoms.)
Example: Clotting
Consider blood clotting. Since very early in this pandemic, science has known that microclots are a common and significant effect of infection with SARS2.
Blood tests can show whether you have elevated d-dimer. If you do, you and your doctor can start treatments to address too much clotting in your blood. It’s reasonable to suspect that if this is still a problem months after you “recovered” from COVID, maybe the virus is still hiding out somewhere inside you and keeping the trouble from being resolved. Getting rid of the virus completely would open the possibility of eventually making the microclot problem go away.
However, you can’t afford to wait until you have finished exploring that. Clots can starve parts of your body of the oxygen they need to function. If they block an essential blood vessel in a critical location, they can kill you quickly.
Your doctor has an arsenal of drugs to address clotting. (I won’t try to list them. The list keeps changing.) Blood thinners won’t be enough because the clots can occlude or completely block blood vessels. Some medications can help your body dissolve clots as they form, which you need if you’ve got microclots.
If you don’t have reasonably good access to a doctor who is willing to help you do this, there are over the counter substances you can use to address clotting and blood flow. They probably won’t be as potent and you’ll have to pay attention to how they interact.
For example, I take feverfew and turmeric for their anti-inflammatory properties. They also lengthen clotting times, as a “blood thinner” does. But they don’t dissolve clots. If I had microclots, I would want to try serrapeptase, which has other anti-inflammatory properties and can dissolve some microclots. To do that, I would have to make a choice. Taking them all would extend my clotting times too much to be safe. I would need to at least not take turmeric when I took serrapeptase.
Wrapping Up
Of the categories:
You can do something about clotting behavior.
You may be able to do something about viral persistence, which will improve everything if you can knock the virus down.
My personal suspicion is that cardiovascular problems with structure and transport are related to viral persistence and to a lesser extent to inflammation. If that’s happening, you’ll need to knock down virus levels to give your body a chance to heal cardiovascular structure and transport.
Cardiovascular operational management involves the central nervous system and autonomic systems. That will be part of the next topic in this series. Buckle up because that’s a wild ride.
The next post in this series is After Getting COVID, Part 5.
Note: This post was lightly edited 2024-06-18.




I should have mentioned, the UK where I live mostly tries to pretend the pandemic is over, but the NHS does not accept blood donations from people who have had COVID until at least 6 months after all symptoms are gone. Viral persistence is a major concern. So far attempting to kick the virus generally involves the same treatments as for the initial acute infection: Paxlovid, ensitrelvir, metformin (or berberine if you can't get your hands on medications), protease inhibitors normally used against HIV, etc.